There is a video on their website that shows how cell replication is interrupted by the alternating tumor treating fields: http://www.novocure.com/ttf_therapy.php?ID=16 It uses some technical jargon but only lasts a minute and a half, and the picture shows how the cells have trouble replicating. Since cancer cells replicate much faster than normal cells, they are more sensitive to the TTF than normal cells, and therefore able to die off more quickly.
On Thursday, 10/25/14, they had a Novocure representative at their house who spent about 3 hours training them in their new equipment. Dr. Hu made a map of where to place the electrode arrays on Steve's head. We understand the location often changes after MRIs based on changes in the tumor.
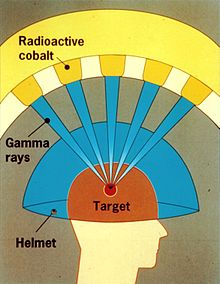
 |
| Electode array |
 |
| The whole shebang |
Steve said he initially felt a warm tingling sensation when the unit was first put on, but now he does not feel anything. The doctor wants Steve to wear the device on average 20 hours per day, or 80% of the day. Steve's first week averaged 85%. There is always some time when the unit is off every day: showers, head re-shaving, when the electrodes are not making good contact or are being replaced every 3-4 days.
Our sister, Lesley told me Steve's personal goal is to wear the machine 95% of the time. She said he has an excellent outlook on the whole thing since he said "this machine is keeping me alive so I'm just going to live with it". And then he picks up all the cumbersome equipment and carries it around with him, even a million times to answer the door for trick or treaters, or to get on the treadmill. They have learned to braid the wires on the right side of his head so they don't tangle when the bag is on the passenger seat of the car. Steve wears a baseball cap most of the time to cover the arrays.
So far, Steve has not had any side effects. The typical side effect is irritation of the skin under the electrodes. He has a cortisone cream for when that happens. It would be applied for 10 minutes, then wiped off with alcohol so the arrays would re-stick to his head. He's not even had any pain when the tape is pulled off or when being shaved down to bare skin :)
Compared to chemotherapy the side effects are nearly inconsequential. With Temodar, he had nausea, needing meds, constipation, needing meds, serious kidney problems and then he had to stop taking it in August because his blood platelets got too low. With Avastin, he had a life-threatening blood clot with leg pain, now needing twice a day shots in his stomach and he gets diarrhea and feels cold very easily.
There are lots of other side effects which could be serious, too and we worry about "chemo brain" over time. Lesley said Steve's stomach looks horrible from all the bruising from the blood thinner shots. He looks like got beat up and lost. Terry does that to him, LOL.
So that's the current news on the Novocure device. I'm looking forward to seeing a picture of Steve with it on and will pass it on to you when I do.